News
‘Better Together with Integrated Care’ report recommends partnering to care for people with SMI
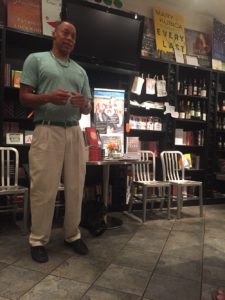
Track star Julius Mercer, who receives integrated primary and mental-health care from Tapestry 360 Health and Trilogy Behavioral Health Care, is now an author and inspirational speaker. A new report highlights Heartland’s integrated care for people with SMI.
Julius Mercer says support of family and friends helped him become a track and field All-American in the 1980s, alongside stars like Carl Lewis.
Inflammation in his knees stopped Mercer from reaching the Olympics. Then, his life unwound due to an untreated bipolar affective disorder that led to substance abuse, then four years in prison.
Since 2014, Mercer has benefited from integrated care delivered by social workers from Trilogy Behavioral Healthcare and primary-care providers from Tapestry 360 Health.
Mercer’s story is part of a new report from Heartland, Better Together with Integrated Care: The Difference for People with Serious Mental Illness that documents the value of integrated care and recommends changes to further the spread of integrated care for people with Serious Mental Illness, SMI.
Tapestry 360 Health provides primary care right in the facilities of partners Trilogy, Thresholds and Community Counseling Centers Chicago. From checkups to psychiatry to shared medical records, we collaborate intensively.
Integrated care is helping people with SMI
It’s working! We’ve found many patients who receive integrated care do better on weight loss, smoking cessation, blood pressure and other indicators, while patients’ satisfaction with their care increased.
Over 1,000 clients participated in Trilogy Heartland Integrated Healthcare program over the last four years. Of clients who completed the NOMs (National Outcome Measures) assessments:
- 47% have an improved BMI (weight management)
- 44% have an improved HgBA1C (diabetes management)
- 58% have improved cholesterol
- 18% have improved blood pressure
- 36% have improved Breath CO level (smoking cessation)
But care integration for people with serious mental illness remains rare in Illinois and beyond. We decided to produce a report on what’s working and including recommendations on how to strengthen integrated care in Illinois.
How it works–and how to improve
The report highlights three key components to know about integrated care:
1) Extra time and sensitivity is required to get results for patients with SMI
Dr. Laurie Carrier, a psychiatrist and family-medicine specialist who serves as medical director at Tapestry 360 Health, says she and other providers tend to see patients with SMI more often – 9 to 11 visits a year on average compared to 2 to 3 visits a year on average for all patients — and spend a bit longer at each visit to build rapport.
2) Primary & behavioral health care partners must team up to improve patient outcomes
Team-based care for each patient can make a big difference. For example at Trilogy Behavioral Health Care, pharmacy is also onsite, so those prescribing and filling prescriptions can compare notes on each patient’s medications.
3) Shared values and coordination at the top drive integrated care partnerships
Agency leaders from Trilogy, Thresholds and Tapestry 360 Health meet regularly to coordinate their efforts and insure partnerships are working as envisioned.
In addition, the report offers two recommendations:
4) New measures to evaluate and share effectiveness would support integration
More visits and services can increase expense to care for people with SMI, but it can also reduce emergency room visits and prevent expensive interventions, which lowers overall per-patient costs. If insurers in Illinois provided per-patient data, it would help medical providers evaluate and demonstrate savings from integrated care.
5) Integrated care funding and reimbursement formulas and methods need improvement
Reimbursement to primary and mental health centers is disjointed, with each getting reimbursed for similar services at differing rates, via different billing methods and codes.
The report also highlights results of integrated care partnerships including results from a federal demonstration program that supported Heartland-Trilogy integrated care.
Mercer’s integrated care
Between appearances as an inspirational speaker and self-published author, Mercer visits Trilogy-Heartland weekly to check in. While there he can see his therapist, pick up his prescription at the on-site pharmacy, and see his medical provider.
His high-cholesterol spurred the former athlete to take Zumba classes and put himself on a diet. “I dropped 13 pounds in the past nine months,” he says.
Download the full report here. Thank you for reading! We welcome your comments, let us know your thoughts via our Contact Form.
Background: Facts about behavioral health on the North Side
On Chicago’s North Side and nearby suburbs where Tapestry 360 Health works, there were 60,031 behavioral health hospitalizations in 2011, almost twice as many as for heart disease (33,689). This is according to the city’s Healthy Chicago 2.0 report.
Studies show immigrants, like many who live in our service area, access care at rates below the general population, leaving them at risk of untreated mental health conditions.
Community-based care for people with SMI is a growing need. Medicaid expansion and the move to managed care have driven expanded primary care coverage for many in Illinois. The Ligas, Williams and Colbert consent decrees are driving a parallel expansion of demand for community mental health services here. In these three cases, federal judges upheld the right of individuals with disabilities to live in the community.
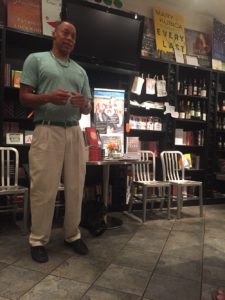
Track star Julius Mercer, who receives integrated primary and mental-health care from Tapestry 360 Health and Trilogy Behavioral Health Care, is now an author and inspirational speaker. A new report highlights Heartland’s integrated care for people with SMI.
Julius Mercer says support of family and friends helped him become a track and field All-American in the 1980s, alongside stars like Carl Lewis.
Inflammation in his knees stopped Mercer from reaching the Olympics. Then, his life unwound due to an untreated bipolar affective disorder that led to substance abuse, then four years in prison.
Since 2014, Mercer has benefited from integrated care delivered by social workers from Trilogy Behavioral Healthcare and primary-care providers from Tapestry 360 Health.
Mercer’s story is part of a new report from Heartland, Better Together with Integrated Care: The Difference for People with Serious Mental Illness that documents the value of integrated care and recommends changes to further the spread of integrated care for people with Serious Mental Illness, SMI.
Tapestry 360 Health provides primary care right in the facilities of partners Trilogy, Thresholds and Community Counseling Centers Chicago. From checkups to psychiatry to shared medical records, we collaborate intensively.
Integrated care is helping people with SMI
It’s working! We’ve found many patients who receive integrated care do better on weight loss, smoking cessation, blood pressure and other indicators, while patients’ satisfaction with their care increased.
Over 1,000 clients participated in Trilogy Heartland Integrated Healthcare program over the last four years. Of clients who completed the NOMs (National Outcome Measures) assessments:
- 47% have an improved BMI (weight management)
- 44% have an improved HgBA1C (diabetes management)
- 58% have improved cholesterol
- 18% have improved blood pressure
- 36% have improved Breath CO level (smoking cessation)
But care integration for people with serious mental illness remains rare in Illinois and beyond. We decided to produce a report on what’s working and including recommendations on how to strengthen integrated care in Illinois.
How it works–and how to improve
The report highlights three key components to know about integrated care:
1) Extra time and sensitivity is required to get results for patients with SMI
Dr. Laurie Carrier, a psychiatrist and family-medicine specialist who serves as medical director at Tapestry 360 Health, says she and other providers tend to see patients with SMI more often – 9 to 11 visits a year on average compared to 2 to 3 visits a year on average for all patients — and spend a bit longer at each visit to build rapport.
2) Primary & behavioral health care partners must team up to improve patient outcomes
Team-based care for each patient can make a big difference. For example at Trilogy Behavioral Health Care, pharmacy is also onsite, so those prescribing and filling prescriptions can compare notes on each patient’s medications.
3) Shared values and coordination at the top drive integrated care partnerships
Agency leaders from Trilogy, Thresholds and Tapestry 360 Health meet regularly to coordinate their efforts and insure partnerships are working as envisioned.
In addition, the report offers two recommendations:
4) New measures to evaluate and share effectiveness would support integration
More visits and services can increase expense to care for people with SMI, but it can also reduce emergency room visits and prevent expensive interventions, which lowers overall per-patient costs. If insurers in Illinois provided per-patient data, it would help medical providers evaluate and demonstrate savings from integrated care.
5) Integrated care funding and reimbursement formulas and methods need improvement
Reimbursement to primary and mental health centers is disjointed, with each getting reimbursed for similar services at differing rates, via different billing methods and codes.
The report also highlights results of integrated care partnerships including results from a federal demonstration program that supported Heartland-Trilogy integrated care.
Mercer’s integrated care
Between appearances as an inspirational speaker and self-published author, Mercer visits Trilogy-Heartland weekly to check in. While there he can see his therapist, pick up his prescription at the on-site pharmacy, and see his medical provider.
His high-cholesterol spurred the former athlete to take Zumba classes and put himself on a diet. “I dropped 13 pounds in the past nine months,” he says.
Download the full report here. Thank you for reading! We welcome your comments, let us know your thoughts via our Contact Form.
Background: Facts about behavioral health on the North Side
On Chicago’s North Side and nearby suburbs where Tapestry 360 Health works, there were 60,031 behavioral health hospitalizations in 2011, almost twice as many as for heart disease (33,689). This is according to the city’s Healthy Chicago 2.0 report.
Studies show immigrants, like many who live in our service area, access care at rates below the general population, leaving them at risk of untreated mental health conditions.
Community-based care for people with SMI is a growing need. Medicaid expansion and the move to managed care have driven expanded primary care coverage for many in Illinois. The Ligas, Williams and Colbert consent decrees are driving a parallel expansion of demand for community mental health services here. In these three cases, federal judges upheld the right of individuals with disabilities to live in the community.